the inflammation seen in colitis.
Doctors will look at your symptoms closely to separate these conditions and make sure you get the right treatment. Knowing how the diagnosis works can help you work better with your healthcare team.
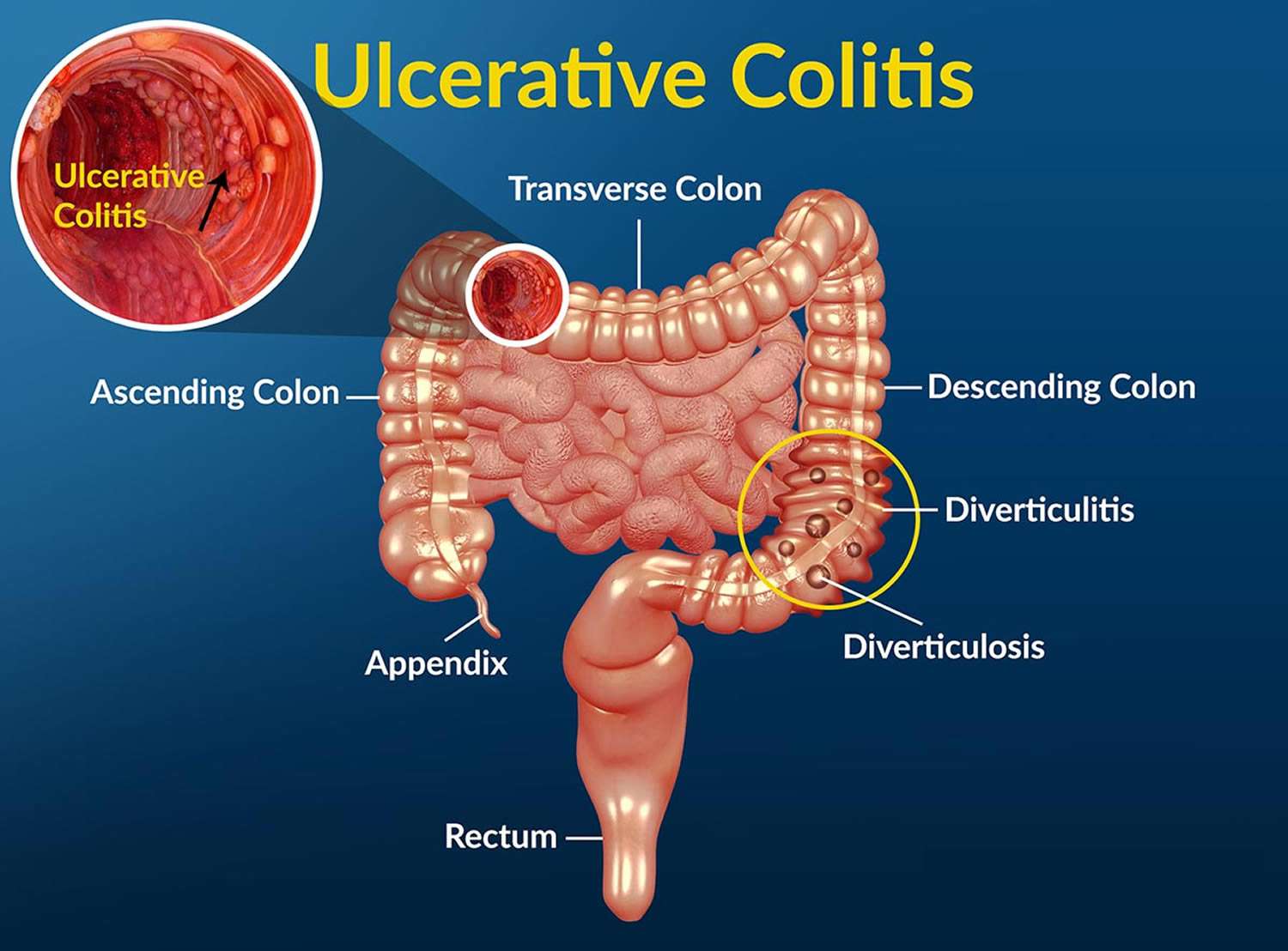
Source: www.bioxcellerator.com
Treatment Options for Ulcerative Colitis
Medications
Treating ulcerative colitis varies from person to person but mainly focuses on managing inflammation and regulating the immune system. Medications are key to relieving symptoms and achieving remission. Here are common types used:
- 5-Aminosalicylic Acid (5-ASA) : First-line treatments like mesalamine help ease inflammation during mild to moderate flare-ups and can be used long-term.
- Corticosteroids : For more severe symptoms, corticosteroids like prednisone are prescribed to reduce inflammation quickly but are only for short-term use due to possible side effects.
- Immunosuppressants : These drugs lower immune activity but take time to work and require regular blood tests to watch for side effects.
- Biologics : Target specific parts of the immune response for moderate to severe cases. They can be given via infusions or injections, often after trying other treatments first.
- JAK Inhibitors : Newer oral medications like tofacitinib focus on blocking certain enzymes tied to inflammation, especially for those who haven’t found relief with usual treatments.
Surgical Interventions
Sometimes, if symptoms are severe or complicated, surgery may be needed. Here’s a look at the options:
- Colectomy : This is when a doctor removes the colon, which can be necessary if other treatments don’t work or significant complications arise.
- Ileostomy : Creating an opening on the abdomen for waste when the colon is removed. Many adapt well to this change.
- Ileoanal Pouch (J-Pouch) : This makes a pouch from the small intestine attached to the anus while letting people have more normal bowel function.
Deciding on surgery is a big deal, so it's good to discuss all the risks and benefits with your healthcare team to feel confident in managing ulcerative colitis while keeping your quality of life.
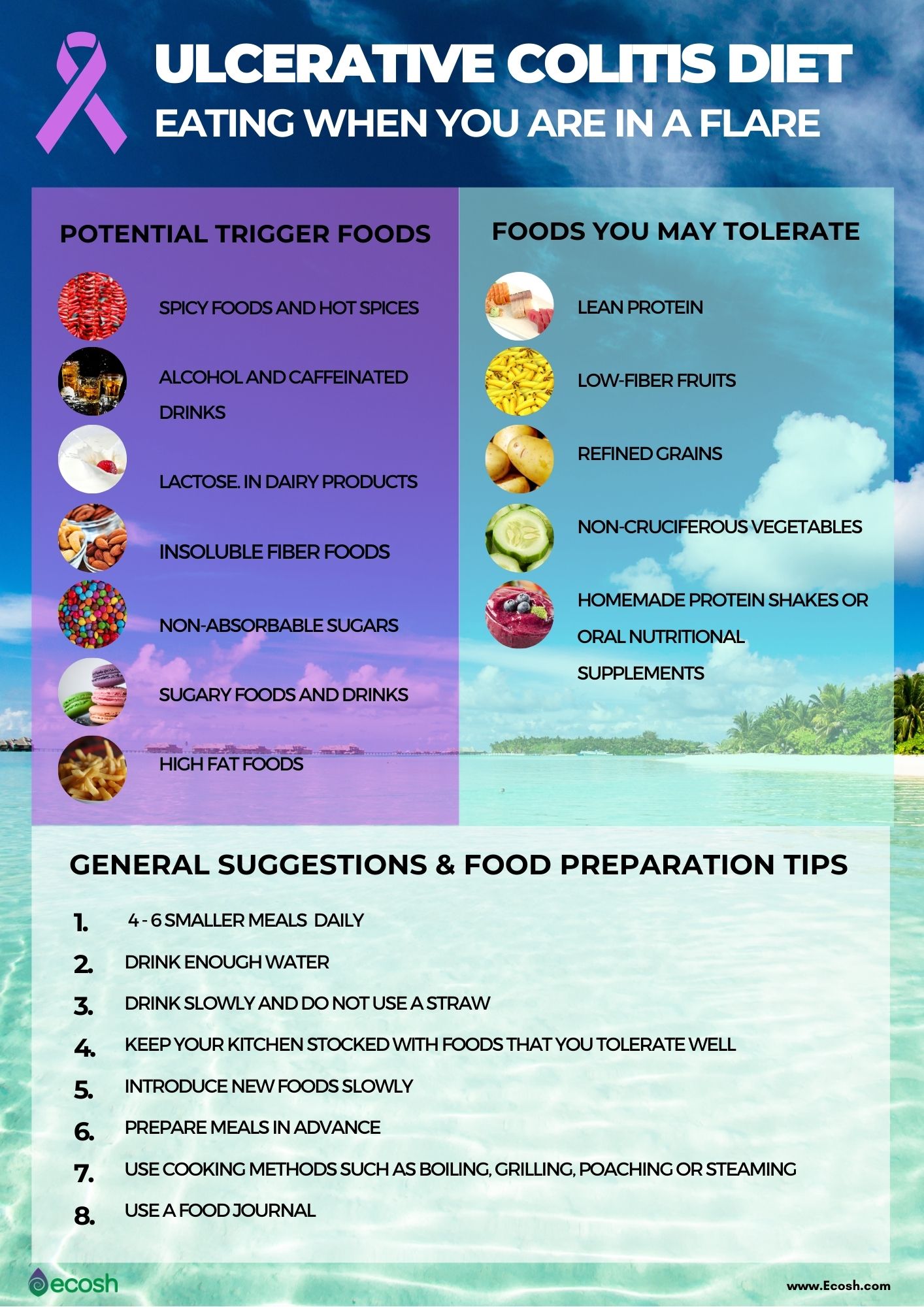
Source: ecosh.com
Lifestyle Changes for Managing Ulcerative Colitis
Diet and Nutrition
Taking care of ulcerative colitis often starts with being mindful about what you eat. There’s no universal diet that works for everyone, but making smart food choices can help ease symptoms. Here are some practical tips:
-
Identify Problem Foods : Keep a food diary to see what you eat and how it makes you feel. Common irritants could be:
- High-fiber foods : Nuts, seeds, corn, and popcorn may worsen symptoms.
- Dairy products : Many find that cutting down on milk, cheese, and yogurt can help reduce discomfort.
-
Incorporate Soft Foods : When symptoms flare up, stick to soft, bland foods that are easier to digest. Cooking methods like steaming or baking can keep nutrients while making things gentler on your stomach.
-
Eat Smaller, Frequent Meals : Instead of three large meals, try five to six smaller ones throughout the day to help manage your symptoms.
-
Stay Hydrated : Drink lots of water, and try to limit carbonated drinks and alcohol, as these can worsen your symptoms.
Stress Management Techniques
While stress doesn't cause ulcerative colitis, it can definitely make things worse. Here are some effective ways to manage stress:
-
Regular Exercise : Activities like walking, cycling, or yoga can really help bring down stress levels and improve your mood.
-
Mindfulness and Relaxation : Things like meditation or deep-breathing exercises can help calm your mind and possibly lessen triggers for flare-ups.
-
Support Networks : Connecting with others who understand your situation can be super comforting. Whether through local groups or forums online, swapping stories can alleviate feelings of loneliness and provide useful tips.
Combining dietary changes with stress management can help you take better control of your symptoms and well-being, making it easier to face life’s challenges.
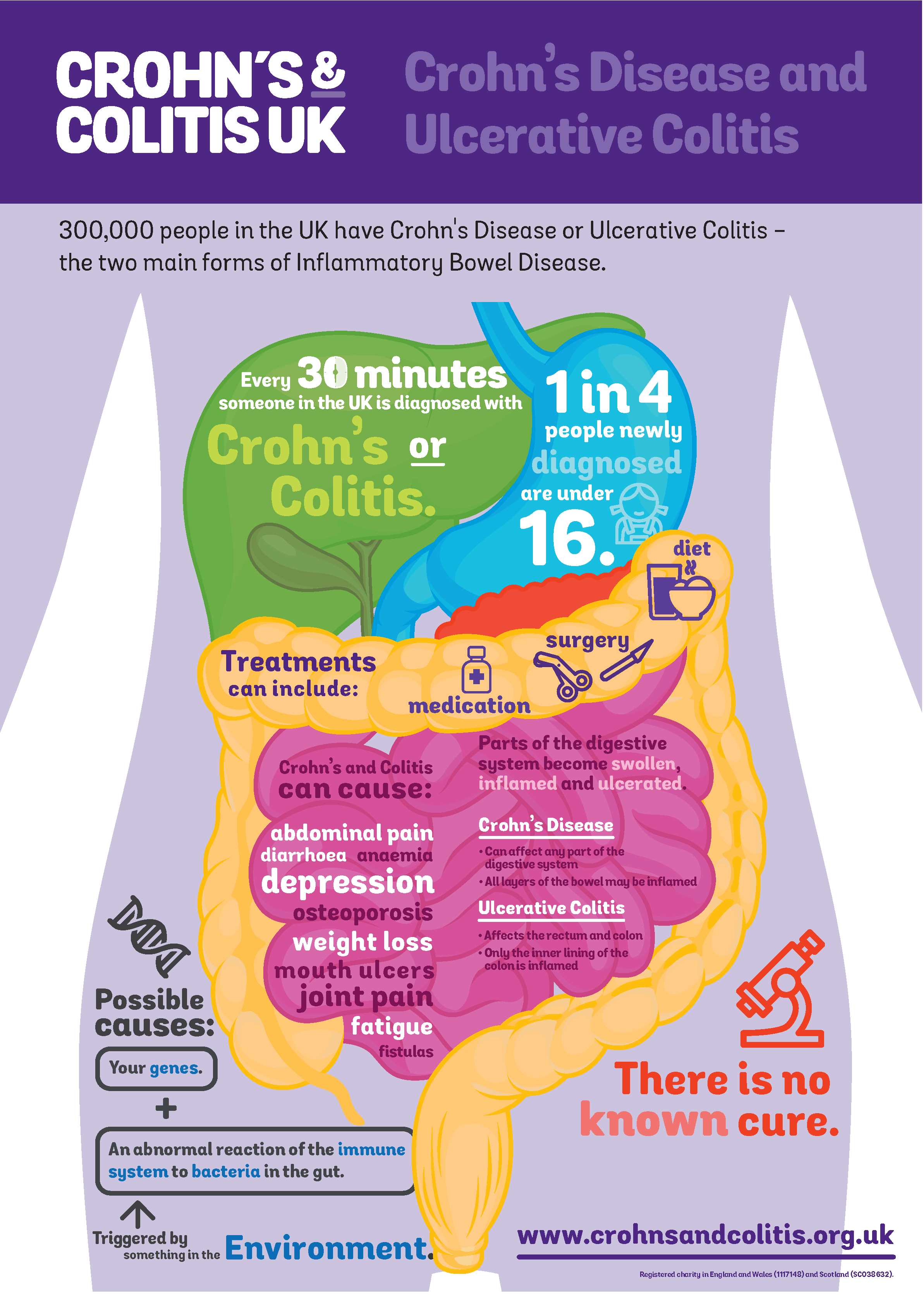
Source: crohnsandcolitis.org.uk
Support Systems for Individuals with Ulcerative Colitis
Building a Healthcare Team
Navigating ulcerative colitis can be tough, and having a reliable healthcare team is essential. Here’s who can be part of that team:
-
Gastroenterologists : These specialists know a lot about inflammatory bowel diseases and can offer personalized treatment plans.
-
Dieticians : Nutritionists who focus on gut health can help create diets that keep your symptoms in check and ensure you're getting the right nutrients.
-
Mental Health Professionals : Living with a chronic condition can take a toll on your emotional health. A therapist experienced with chronic illnesses can share coping strategies.
-
Primary Care Physicians : Regular check-ups can help manage any other health concerns that come up alongside UC.
Good communication with your healthcare team helps you set goals and track progress, and it’s okay to voice concerns or ask questions!
Joining Support Groups
Support groups can be a great source for both resources and camaraderie, making you feel less alone in your journey with UC. Here’s how joining can help:
-
Shared Experiences : Connecting with others who are going through similar challenges can lead to a sense of community and understanding. It’s valuable to hear different coping strategies from people in the same boat.
-
Access to Info : Many groups offer up-to-date resources about managing UC, new treatments, and dietary tips.
-
Tailored Support : There are support groups for various demographics, including college students and older adults, so you can find a community that fits your situation.
Whether you join local support groups or connect with others online, having a network of caring individuals can make a significant difference in your journey managing ulcerative colitis. This support system empowers you to tackle your health journey confidently, knowing you're not alone.

Source: blackdoctor.org
Pregnancy and Ulcerative Colitis
Potential Risks and Challenges
Pregnancy sure can be an exciting time, but if you have ulcerative colitis (UC), it can also bring some unique risks and challenges. While many women with UC have normal pregnancies, if the condition is active during pregnancy, there are some complications to consider:
-
Increased Pregnancy Problems : If UC is active, it may raise the chances for issues like gestational diabetes or preterm birth, so effectively managing UC before and during pregnancy is important.
-
Flare-Ups : The stress of pregnancy might trigger symptom flare-ups, complicating matters further. Being aware of how UC interacts with pregnancy can help you navigate these changes.
-
Medication Management : Some UC medications may be unsafe during pregnancy. It’s essential to consult your doctor about any medications you’re taking to make sure they're safe for you and the baby.
Connecting with other moms who have been through similar situations can offer emotional support and practical tips for managing these challenges.
Managing the Condition During Pregnancy
To successfully manage ulcerative colitis while pregnant, solid care and proactive strategies are key. Check out these suggestions:
-
Preconception Planning : Before trying to conceive, chat with your care team to make sure your UC is in remission to help minimize potential issues.
-
Regular Monitoring : Keep in touch with your healthcare team to keep an eye on your UC throughout the pregnancy. Regular visits can help adjust treatment as needed.
-
Nutrition : Following a balanced diet rich in vitamins and minerals is vital. Working with a dietitian to create a meal plan that meets your nutritional needs is a smart move.
-
Stress Management : Adding relaxation techniques like yoga or meditation can help lower stress, which is key for managing both UC and pregnancy.
With the right support and proactive approaches, those with ulcerative colitis can have healthy pregnancies while safeguarding their well-being. Working closely with healthcare providers and tapping into community resources can make the journey smoother.

Source: m.media-amazon.com
Work and Social Life with Ulcerative Colitis
Communication Tips with Employers
Managing ulcerative colitis in the workplace can be tricky, but being open with your employer is important. Here are some handy tips to kick off those conversations:
-
Be Honest but Thoughtful : If you’re comfortable, talk to HR or your supervisor about your condition. You don’t need to go into all the details; just mention how it might occasionally affect your work. Try saying something like, "I have a health condition that can impact my availability."
-
Know Your Rights : Get to know your workplace rights regarding chronic illnesses. Many places have laws protecting employees from discrimination based on health issues, which can empower you in discussions with your employer.
-
Suggest Solutions : Think ahead and offer up ideas for solutions while discussing your needs. If flexibility during flare-ups would help, suggest a plan that works for both you and your job.
-
Keep the Communication Open : Letting your employer know about any changes in your condition can promote understanding and support. Regular check-ins can clarify expectations on both sides.
Balancing Social Activities
Having an active social life is important for mental health, but it often takes some careful coordination when managing ulcerative colitis. Here are some ways to strike that balance:
-
Choose Activities Wisely : Pick social events that match how you're feeling. If you’re good to go, join friends for light outings. If your symptoms are acting up, suggest low-key activities like a movie night at home.
-
Plan Ahead : Before heading out to an event, check where restrooms are located, especially if you're worried about your symptoms. Many airports have online maps for restroom locations.
-
Be Honest with Friends : Sharing your experiences can lead to unexpected support. Telling a close friend about your UC might result in increased understanding and empathy.
-
Take Breaks When Needed : It’s completely fine to step away from a social situation if you’re feeling overwhelmed. Take time to recharge and put your health first when you need it.
Through open communication and thoughtful planning, individuals with ulcerative colitis can have satisfying work and social lives, ensuring that their condition doesn’t define their experiences. Always remember, you’re more than your diagnosis!

Source: www.fomatmedical.com
Research and Advancements in Ulcerative Colitis
Current Studies and Findings
Recent research in ulcerative colitis (UC) has shown impressive advancements in understanding the disease and its management. Here are some highlights from key studies:
-
Epidemiology Insights : Globally, there's been a concerning rise in UC cases, especially in newly industrialized countries. This calls for better awareness and healthcare resources to effectively manage the condition.
-
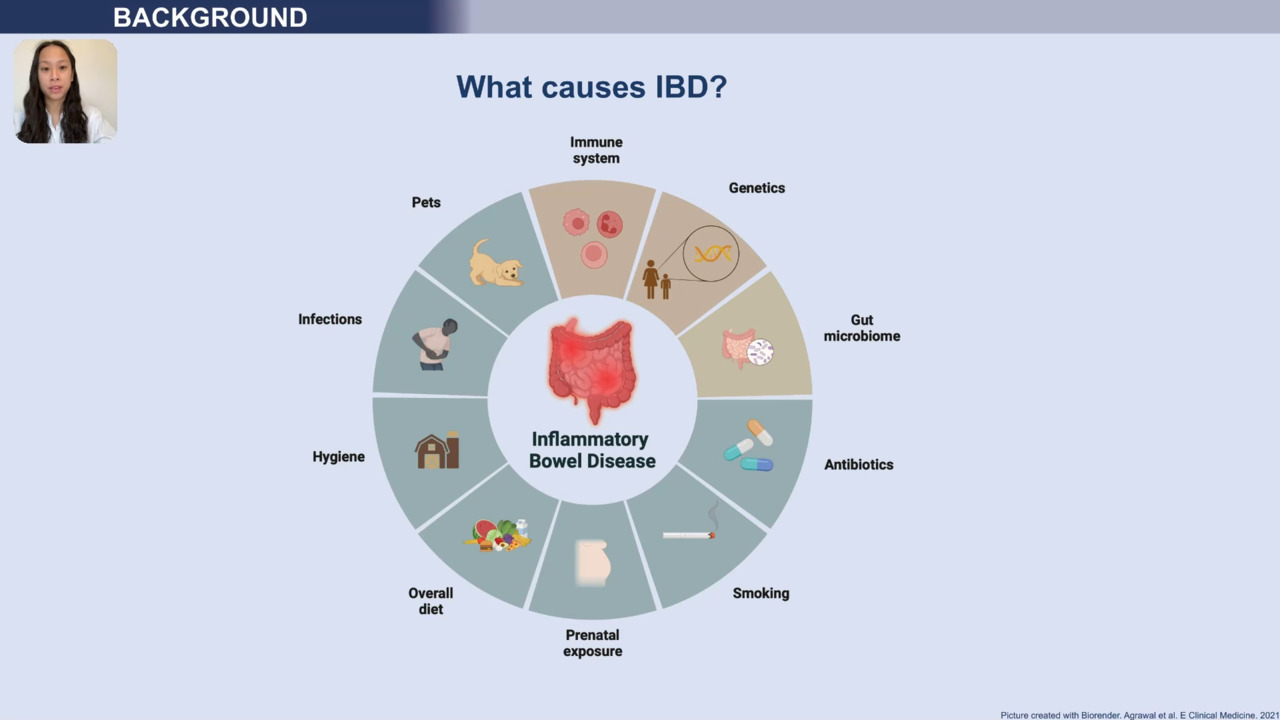
Pathophysiology : Studies show that UC’s complexity involves genetic, environmental, and immune factors. Knowing more about these can help find potential biomarkers for early diagnosis and tailored treatments.
-
Diagnostic Advancements : New imaging technologies like magnetic resonance enterography and capsule endoscopy offer enhanced visualization of the gastrointestinal tract, which aids in spotting inflammation and strictures.
Researchers continue working hard to improve diagnostic methods, which is essential for starting timely and effective treatments.
Promising Treatment Approaches
The treatment options for ulcerative colitis are promising, showing advancements in medications and therapies:
-
Biologics and Targeted Therapies : Treatments like infliximab and adalimumab target specific inflammatory pathways, changing how UC is managed. Studies show that these not only help with symptoms but also lead to mucosal healing and long-term remissions.
-
JAK Inhibitors : New oral medications like tofacitinib are proving effective for patients who didn’t respond well to traditional therapies.
-
Personalized Medicine : Research into genetic factors and individual responses is paving the way for more customized treatments, aimed at boosting effectiveness while cutting down side effects.
-
Nutritional Interventions : There's increasing awareness of how nutrition plays a role in managing UC, with certain diets and supplements being studied for their potential benefits.
Through ongoing research and innovative treatment methods, there’s hope for people with ulcerative colitis to enjoy better quality of life and improved management of their condition. Staying updated on these advancements helps patients interact more effectively with their healthcare providers to find the best plan for their unique needs.
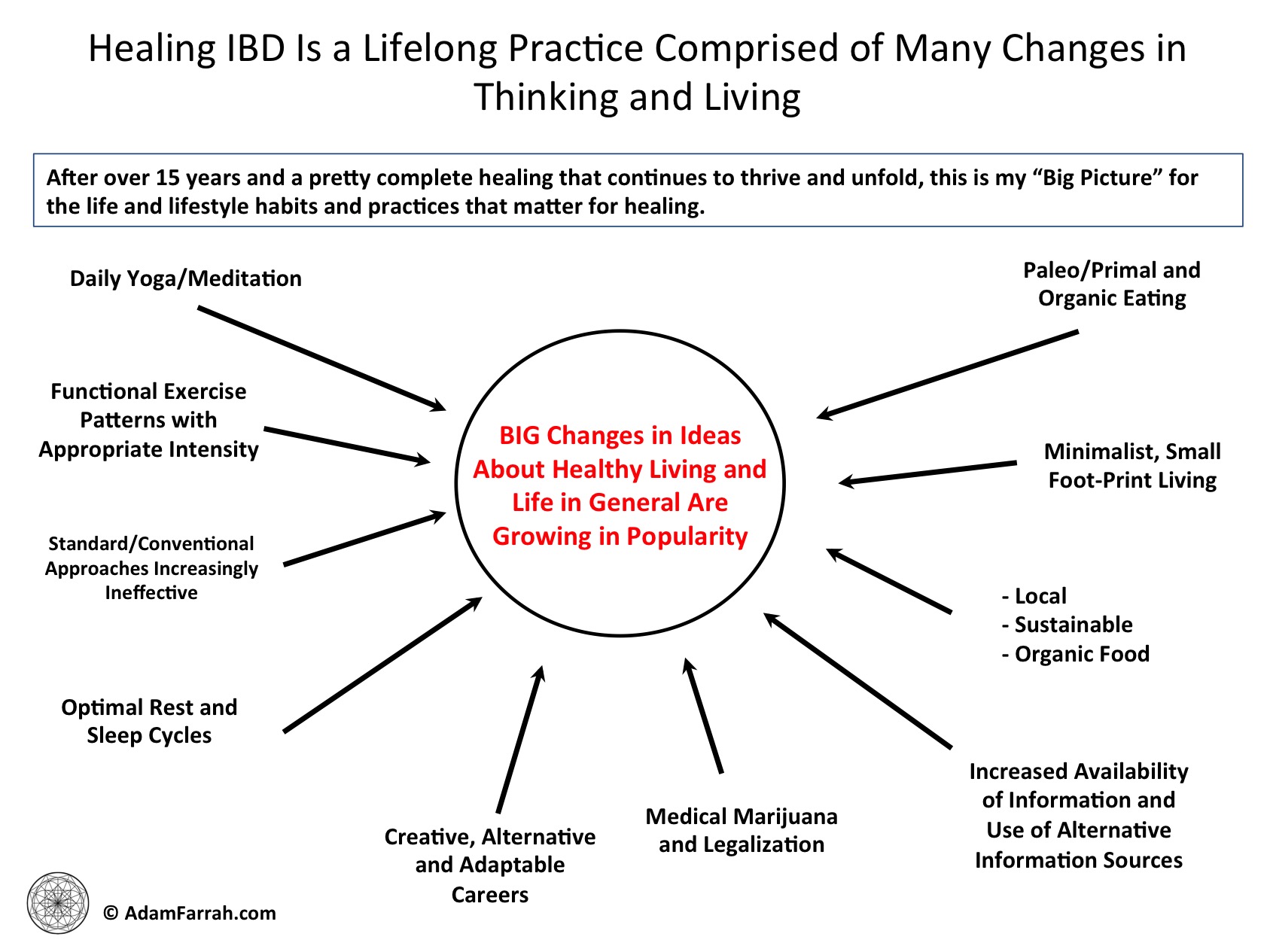
Source: adamfarrah.com
Coping Strategies for Flare-Ups
Dealing with Pain and Discomfort
Flare-ups of ulcerative colitis can be tough and uncomfortable. Knowing how to cope with the pain and symptoms can really help manage your condition better. Here are some strategies that can make a difference:
-
Stay Hydrated : Dehydration can make symptoms worse, so drink plenty of water throughout the day. Herbal teas and clear broths can also be soothing.
-
Heat Therapy : Using a heating pad on your belly can relieve cramps and discomfort. Lots of people find warmth comforting during flare-ups.
-
Diet Adjustments : When you’re having a flare, consider sticking to a low-fiber diet. Foods like bananas, rice, and cooked veggies are easier on your digestive system. Try to avoid potential irritants like fatty or spicy foods, dairy, and nuts.
-
Rest and Relaxation : Make sure to get enough rest. Stress can make symptoms worse, so engage in calming activities like reading, gentle yoga, or meditation to manage anxiety.
-
Medication : Keep up with your prescribed meds and talk to your doctor if you feel adjustments are needed.
When to Seek Medical Help
While many flare-ups can be handled at home, it's important to know when to reach out for help. Key signs that you should see a doctor include:
-
Persistent Symptoms : If you’re experiencing severe stomach pain, ongoing diarrhea (especially with blood), or rectal bleeding that won’t get better, it’s time to call your doctor.
-
Signs of Dehydration : Symptoms like feeling dizzy, having a dry mouth, or urinating less are signs of dehydration that may need treatment.
-
Fever or Chills : If you have a fever along with worsening UC symptoms, it could be a sign of an infection or serious inflammation, which needs medical review.
-
Impact on Daily Life : If flare-ups are seriously affecting your ability to work, socialize, or enjoy life, discuss this with your healthcare team to revise your management plan.
By using coping strategies and keeping an eye on symptoms, you can handle flare-ups and maintain a good quality of life. Regularly communicating with your healthcare team is key to managing this chronic condition effectively.

Source: www.gastrojournal.org
Understanding the Psychological Impact of Ulcerative Colitis
Mental Health Considerations
Living with ulcerative colitis (UC) isn’t just about managing physical symptoms; it has significant psychological effects as well. Studies show that those with UC often experience higher levels of anxiety and depression compared to those without the condition. The unpredictability of flare-ups can create feelings of helplessness and stress, which might worsen symptoms and create a vicious cycle.
-
Emotional Effects : It’s normal to feel anxious about bathroom access or fear of abdominal pain during social situations. This kind of stress can lead to avoiding activities you used to love, impacting your quality of life.
-
Body Image Issues : Symptoms like bloating or weight changes can affect how you see your body, making it crucial to address the mental health side of living with UC.
Recognizing these emotional challenges is important since they can influence medication adherence and day-to-day activities. Understanding that UC affects both body and mind encourages seeking support for mental health along with physical symptoms.
Seeking Therapy and Counseling
Getting professional help can add valuable support when managing the psychological effects of ulcerative colitis. Here are some helpful resources:
-
Cognitive Behavioral Therapy (CBT) : This kind of therapy can help change negative thought patterns related to UC, assisting with stress and anxiety management.
-
Gut-Directed Hypnotherapy : This approach may ease gastrointestinal symptoms while also addressing emotional health.
-
Support Groups : Talking with others who share similar experiences can foster understanding and community. Sharing your journey with those who truly get it can be incredibly healing.
Remember that seeking help is a proactive way to enhance your overall quality of life. Talk to your doctor about mental health resources available near you. Working with a mental health professional can provide tools and strategies to tackle the complexities of ulcerative colitis, helping you lead a fuller life despite the condition.

Source: i0.wp.com
Traveling with Ulcerative Colitis
Preparing for Trips
Traveling with ulcerative colitis (UC) is totally doable with some smart preparation. Here are key strategies to make your trip go smoothly:
-
Consult Your Doctor : Before you head out, chat with your healthcare provider. They can point out any specific medical considerations related to your case and may provide a letter explaining your condition and medications.
-
Pack Wisely : Create an emergency kit that includes must-haves like:
- Extra medications
- Bathroom supplies (toilet paper, wipes)
- Change of clothes
- Hand sanitizer
- Snacks that are easy on your stomach
-
Book Accommodations Carefully : If possible, choose places with private bathrooms. Having that comfort can really help during your stay.
-
Plan Your Route : Know where the restrooms are along your route, whether you're driving or flying. Most airports offer online resources with restroom maps, which can be super handy.
Managing Symptoms on the Go
While you're traveling, keeping a close watch on your health helps manage symptoms better. Here are some strategies:
-
Stay Hydrated : Drink plenty of water during your trip; staying hydrated is crucial. Having a reusable water bottle makes this easier.
-
Avoid Trigger Foods : Stick to foods you know your body can handle. If uncertain about dishes at restaurants, ask how they’re prepared.
-
Listen to Your Body : If something doesn’t feel right or you sense a flare-up coming, consider slowing down and resting. Taking breaks during busy activities can help you recharge.
-
Communicate : If you’re traveling with others, let them know what’s going on. Their support can be really helpful if you need help managing your condition.
With proper planning and mindfulness, you can enjoy traveling while managing ulcerative colitis. Remember that keeping a positive mindset can really boost your travel experience!

Source: www.irjournal.org
Alternative and Complementary Therapies for Ulcerative Colitis
Herbal Remedies
Some people with ulcerative colitis (UC) find comfort in using herbal remedies alongside their regular treatment. While scientific support is still emerging, many patients have reported relief from certain natural options. Here are a few you might consider:
-
Curcumin (Turmeric) : Known for its anti-inflammatory skills, curcumin might help with UC-related inflammation. Some studies suggest it can work well with standard treatments. If you're thinking of adding curcumin, just make sure to pick high-quality supplements.
-
Aloe Vera : This plant is famous for its calming properties. Some research shows that aloe vera might help reduce inflammation, but for certain people, it can cause diarrhea, so pay attention to how your body reacts.
-
Fish Oil : High in omega-3 fatty acids, fish oil has shown promise in controlling inflammation. Talk to your healthcare provider before adding it to your routine since dosages can vary.
Using herbal remedies may be beneficial, but they shouldn't replace conventional treatments. Always check with your doctor to ensure these supplements play nice with your current medications.
Acupuncture and Mindfulness Practices
Acupuncture and mindfulness have roots in traditional therapies and can add benefits for people with ulcerative colitis:
-
Acupuncture : This ancient technique involves inserting needles at specific body points. Some studies suggest it may reduce UC symptoms like pain and nausea, with many patients feeling relaxed post-session.
-
Mindfulness and Meditation : Emphasizing present-moment awareness may help with stress, a known trigger for UC flare-ups. Practices like deep breathing, yoga, or guided imagery can promote relaxation and benefit your mental health.
-
Cognitive Behavioral Therapy (CBT) : This therapy focuses on identifying and changing negative thought patterns that may arise from living with UC. Many find it helpful for addressing anxiety and depression.
Adding acupuncture and mindfulness to your routine may improve your management of ulcerative colitis. These practices not only support your physical health but also bolster emotional resilience, which is key for managing the condition long-term. Always run any new therapies by your healthcare team to ensure everything aligns.
Source: cf-images.eu-west-1.prod.boltdns.net
Exploring the Connection Between Diet and Ulcerative Colitis
Trigger Foods to Avoid
For individuals with ulcerative colitis (UC), keeping an eye on what you eat can heavily impact how you feel. While triggers can vary among people, there are common foods that tend to make UC symptoms worse:
-
High-Fiber Foods : Fresh fruits, raw veggies, nuts, and seeds might irritate during flare-ups. Consider opting for lower-fiber foods or cooking vegetables to ease digestion.
-
Dairy Products : Many find that dairy products flare their symptoms, so cutting down on milk, cheese, and yogurt, especially if lactose intolerance is at play, could help.
-
Processed Foods and Sugars : Diets high in processed foods, sugary goodies, and unhealthy fats can disturb gut health. Stick to whole foods instead—they're better for you!
-
Spicy Foods : Spices can irritate the digestive system, so milder meals tend to be easier to handle.
Keeping a diary of what you eat can help pinpoint your trigger foods, which can help you adjust your diet to feel better during flare-ups.
Nutritional Tips for a Healthy Gut
Eating a balanced, nutrient-filled diet could promote gut health and help manage ulcerative colitis. Here are some pointers for supporting your overall well-being:
-
Incorporate Non-Dairy Calcium Sources : If you limit dairy, check out alternative calcium sources like tofu, almonds, fortified plant-based milks, and leafy greens.
-
Focus on Omega-3 Fatty Acids : Foods high in omega-3s, like salmon, walnuts, and flaxseeds, are known for their anti-inflammatory effects, which can be great for managing UC.
-
Stay Hydrated : It's essential to drink enough fluids, especially during flare-ups or diarrhea. Aim for nice refreshing water or soothing herbal teas.
-
Eat Smaller Meals : Eating smaller, frequent meals can lessen the stress on your digestive system, making it easier to manage symptoms.
By steering clear of trigger foods and embracing a more balanced diet, folks with ulcerative colitis might feel better and have more control over their symptoms. And remember, consulting a healthcare provider or dietitian for a personalized nutrition plan is always a smart choice!

Source: m.media-amazon.com
Advocacy and Raising Awareness About Ulcerative Colitis
Participating in Fundraising Events
Fundraising events are key for raising awareness and funds for research into ulcerative colitis (UC) along with community support. Getting involved in these events not only helps a good cause but also brings a feeling of belonging. Here’s how you can participate:
-
Walks and Runs : Many organizations like the Crohn’s & Colitis Foundation hold annual walks and runs to fund research. Joining in is a great way to connect with others who share similar experiences.
-
Awareness Campaigns : Participate in local events or awareness months to spread knowledge about UC and promote understanding in your community.
-
Team Up with Friends and Family : Forming groups for charitable events can enhance your efforts. Having your friends and family join in can add a sense of camaraderie while raising necessary funds for UC.
Through these engagements, your contributions can drive research that leads to better treatments and care for those with ulcerative colitis.
Sharing Personal Stories to Educate Others
Sharing personal experiences is a powerful way to raise awareness and tackle stigma around ulcerative colitis. Here’s how to effectively share your narrative:
-
Utilize Social Media : Platforms like Instagram or Facebook let you share your journey and insights about living with UC. Regular updates can connect with a wider audience, encouraging helpful conversations and support.
-
Join Support Groups : Participating in or leading local or online support groups lets you share your experiences. This creates a nurturing space for empathy and solidarity.
-
Advocate for Education : Contact schools, community centers, or health facilities about hosting workshops to bust myths about UC and stress the importance of support.
By fundraising and sharing their stories, folks dealing with ulcerative colitis contribute to building a supportive community while also driving positive change in awareness and treatment of the condition. Embracing advocacy can empower both you and others going through similar situations.
